
What is ANC?
Ante-natal consultation is the comprehensive care of the pregnant woman and the child she is carrying, by qualified personnel in a health facility.
Objectives of antenatal surveillance
- Screening and management of
possible pathologies: arterial
hypertension, anemia, malaria,
syphilis, urinary tract infection, HIV
infection, malnutrition, vitamin and
micronutrient deficiency,
etc - Screening and management of
obstetric complications: uterine
scar, abnormal
presentation, premature rupture
of membranes, multiple
pregnancy, metrorrhagia, etc
- Systematic prevention of
maternal and neonatal tetanus,
anemia, maternal-fetal
transmission of HIV, malaria in
endemic areas, etc - Development of the birth plan,
advice, preparation for
childbirth
Rhythm of antenatal consultations
It is recommended to carry out 4 prenatal consultations during an uncomplicated pregnancy.
If the patient does not present until the sixth month, endeavor to carry out at least 2 consultations before delivery.

First Consultation
A. Questioning
- General feelings about the pregnancy (problems/concerns)
- Social context: family situation, detection of sexual, marital or domestic violence, living
conditions, professional activity, etc. - Date of last menstrual period.
- Obstetrical and surgical history:
• Number of previous pregnancies;
• Complications during previous pregnancies or deliveries (hemorrhage, infection, prematurity,
p. ex.) ;
• Spontaneous or induced abortion(s);
• Living or dead children;
• Cesarean (find out the indication) or any other intervention on the uterus;
• Instrumental extraction;
• Vesicovaginal or rectovaginal fistula. - Vaccination status for tetanus.
- Current complaints: pelvic pain, contractions, fever, urinary disorders, bleeding, abnormal vaginal discharge, etc.
- Medical history and current treatment: hypertension,diabetes, asthma, epilepsy, heart disease, HIV infection, psychiatric disorders, etc.

The age of pregnancy is estimated by counting the number of weeks of amenorrhea (WA) since the first day of the last menstrual period, using a calendar or a pregnancy disc.
For example, if the date of the last menstrual period is December 15, 2018 and the woman is seen on January 27, 2019, the gestational age is estimated at 6 weeks amenorrhea.
Always check that this estimate agrees with the data from the clinical examination (estimate of uterine volume) or ultrasound
The expected date of delivery is estimated by counting 40 or 41 weeks of amenorrhea from the first day of the last menstrual period. For example, if the date of the last period is December 15, 2018, the expected date of delivery is between September 22 and 29, 2019
The expected date of delivery can also be estimated by counting 9 months plus 7 to14 days after the first day of the last menstrual period. If the woman does not know the date of the last menstrual period, the probable age of pregnancy and the expected date of delivery is established from the clinical examination or ultrasound if available
C. Clinical examination
– Weight
– Height (detection of women under 1.50m)
– Blood pressure (patient seated, at rest)
– Search for abdominal scar.
– Search for anemia, edema, etc.
– Search for fetal heart sounds from the end of the first trimester.
– Estimation of uterine volume (allows estimation of gestational age):
• In the first trimester, the uterine volume is assessed by a bimanual examination. At 7 weeks the uterus is the size of a chicken egg, at 10 weeks the size of an orange, at 12 weeks the uterine fundus exceeds the pubic symphysis;
• From the second trimester, the uterus can be perceived by abdominal palpation alone with measurement of the uterine height between the upper edge of the pubic symphysis and the uterine fundus
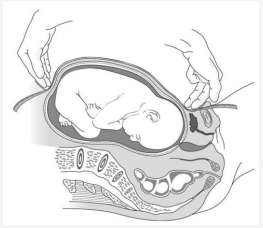
Figure 1.1 -Fundal height measurement
The estimation of gestational age becomes more and more approximate as the pregnancy progresses
| Fundal Height | Amenorrhea weeks |
| 20cm | 18-22 weeks |
| 24cm | 22-26 weeks |
| 28cm | 26-30 weeks |
| 32cm | 30-34 weeks |
| 34cm | 33 weeks at the end |
Table 1.3-Fundal height by term
D. COMPLEMENTARY EXAMINATIONS

Subsequent Consultations
A. Questioning
- Perception by the mother of fetal movements
- Current complaints: pelvic pain, contractions, fever, urinary symptoms, bleeding, abnormal vaginal discharge, etc.
B. Clinical examination
Be careful when examining a woman in the supine position: the weight of the uterus compresses the inferior vena cava, which may cause discomfort (solved by placing the patient in the left lateral decubitus position).

In all cases :
– Blood pressure, weight, edema, fundal height measurement.
– Monitoring of fetal heart sounds: they must be regular, rapid (110 to 160/minute), not synchronous with the maternal pulse.
– Study of the fetal presentation (in the third trimester):
Palpation:
• Cephalic pole: rounded, hard, regular, giving the hands a sensation of sloshing, separated from the rest of the body by the furrow of the neck, beyond which one palpates the projection of the stump of the shoulder.
• Pelvic pole: soft, bulkier and less regular than the cephalic pole, without the presence of the furrow of the neck
Definition of presentation:
• Cephalic: the cephalic pole is in the maternal pelvis.
• Seat: the cephalic pole is in the uterine fundus.
• Transverse: the 2 poles are each in a side.
– Research on the side of the back:
Press down on the uterine fundus to bend the fetal spine and explore the lateral sides of the uterus. The back is palpated like a hard plane, the limbs are perceived as small irregular protrusions. The back is defined in relation to the right or left of the mother.
– In the third trimester, auscultation of fetal heart sounds is performed in the umbilical region, on the side of the back of the fetus, at shoulder level.
Only if indicated:
– Genital examination (for signs of sexually transmitted infections, for example).
– Examination of the vagina (repeated uterine contractions, for example).
Notice :the discovery of a small basin does not predict fetal-pelvic disproportion. It does not justify the programming of a caesarean section. Conversely, a foeto-pelvic disproportion can occur when the pelvis appears normal. In practice, a foeto-pelvic disproportion can only be observed during the evolution of labour.
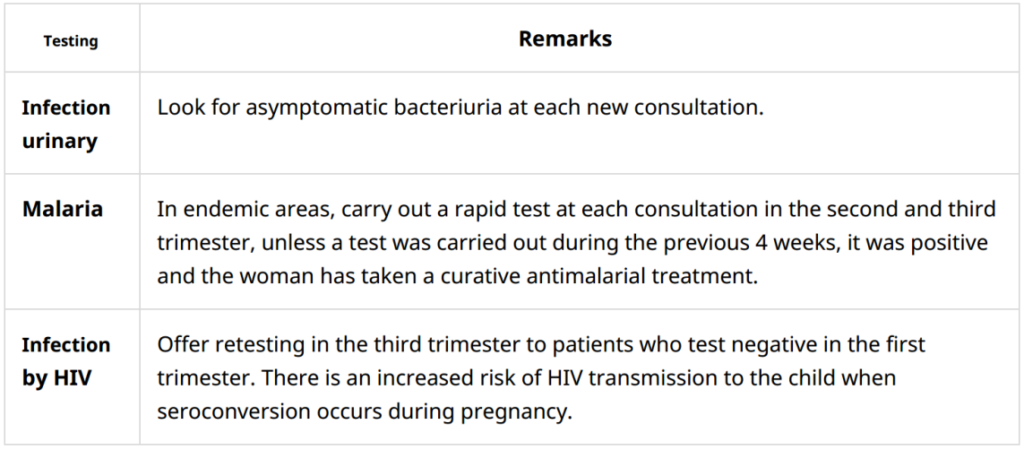
D. Complementary examinations
Systematic Prevention
Maternal and neonatal tetanus
– Pregnant women not vaccinated against tetanus during their childhood or adolescence must receive at least 2 doses of tetanus vaccine (VAT) vs before giving birth:
• the first dose at the first consultation;
• the second dose at least 4 weeks after the first dose and preferably at least 2
weeks before the expected date of delivery in order to optimize the immune response in the mother and the passive transfer of antibodies to the child.
– After delivery, continue according to the scheme below to total 5 doses. Once administered, these 5 doses protect for life.
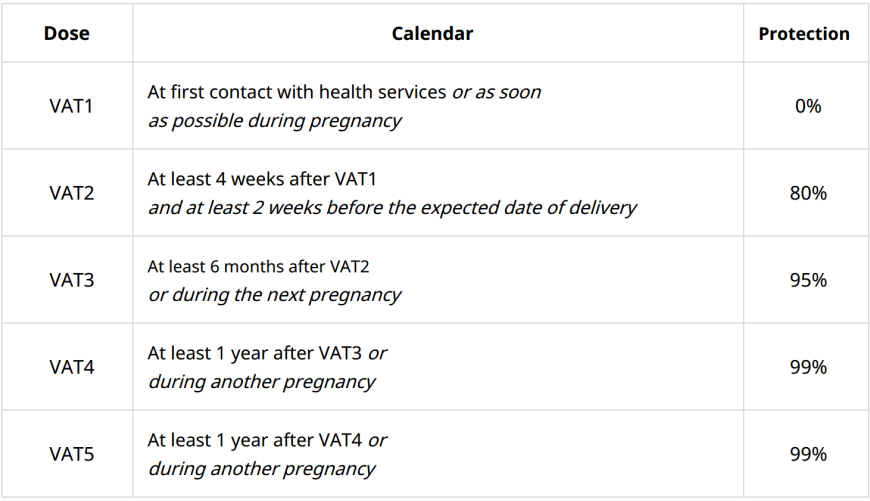
Table 1.6- Vaccination schedule for pregnant women or women of child bearing age
Anemia
1- Absence of anemia
In the absence of clinical or biological signs of anemia:
– Administer iron and folic acid supplementation, starting as soon as possible after the onset of pregnancy and continuing throughout pregnancy, in the form of: ferrous sulphate/folic acid(200 mg tablet of ferrous sulphate i.e. 65 mg of elemental iron + 400 micrograms of folic acid) PO: 1 tablet once a day
Or
multiple micronutrients(93.75 mg tablet of ferrous sulphate or 30 mg of elemental iron + 400 micrograms of folic acid + other nutrients) PO: 1 tablet once a day
In areas where hookworm infection is common (areas with hot and humid climates), also administer antihelminthic treatment from the second trimester:
albendazolePO: 400 mg single dose (ormebendazolePO: 100 mg twice a day for 3 days)
– In areas where malaria is endemic, also administer intermittent preventive antimalarial treatment or curative antimalarial treatment depending on the
results of the screening tests (see below).
Presence of anemia
In the presence of clinical (pale palms, conjunctiva, tongue) or biological anemia (hemoglobin < 11 g/dl in the first and third trimester or < 10.5 g/dl in the second trimester)
Malaria
In all regions where the transmission of malaria to P.falciparumis moderate to strong,prevention is based on:
– The use of mosquito nets impregnated with insecticide (provide 2 mosquito nets).
– Malaria screening at each prenatal consultation in the second and third trimester:
• If the test is positive, whatever the region and whatever the term of the pregnancy:
Administer a curative antimalarial treatment
After a curative treatment, wait a month to repeat a malaria screening test.
• If the test is negative, Intermittent Preventive Treatment (IPT) is recommended in areas of Africa where transmission of malaria from P.falciparumis moderate to strong.
Start an IPT with sulfadoxine/pyrimethamine(MS)[4]from the start of the second trimester. The aim
is to administer at least 3 doses between the second trimester and delivery with an interval of at least 1 month between each treatment. The number of treatments is not
limited as long as an interval of one month is respected between each treatment. The SP dosage for each treatment is 3 single dose tablets. This treatment reduces the consequences of malaria (maternal anemia, low birth weight). Do not administer this intermittent treatment to HIV-infected women on co-trimoxazole
prophylaxis.
Vitamin and micronutrient deficiency
Calcium
Supplementation is recommended for[6]:
• all pregnant adolescents (under 20);
• all pregnant women whose diet is low in calcium AND who present a high risk of pre-eclampsia (history of pre-eclampsia or eclampsia, twin pregnancy, chronic hypertension).
Start supplementation from the first prenatal visit and continue throughout pregnancy:
calcium carbonate PO: one 1.25 g tablet (equivalent to 500mg of elemental calcium per tablet) 3 times a day
Respect an interval of 2 hours between the administration of calcium and iron salts.
– Vitamin D
Sources of vitamin D are exposure to sunlight and food.
Supplementation is considered if there is a risk of deficiency (low exposure to the sun, diet low in vitamin D): cholecalciferol (vitamin D3) or ergocalciferol (vitamin D2) PO: 100,000 IU single dose at 6 or 7 months of pregnancy
– Iodine
Iodine deficiency during pregnancy exposes you to a risk of abortion,
premature delivery, major mental retardation and weight loss in the child, neonatal and infant death. In areas where iodine deficiency is endemic, iodine supplementation is necessary. Comply with national protocol.
B. Estimation of gestational age and expected date of delivery
Malnutrition
– In case of malnutrition, include the woman in a therapeutic nutritional program. If no nutritional program is in place, provide supplementation:
• BP 190-230 mm: 2 sachets of Plumpy’nut or 3 bars of BP100 per day;
• MUAC < 190 mm: 4 sachets of Plumpy’nut or 7 bars of BP100 per day.
– In the absence of signs of malnutrition but in a situation of food shortage, supplement all pregnant women throughout pregnancy.
– In case of overweight or obesity, provide advice to avoid excessive weight gain during pregnancy.
HIV infection
If positive, start antiretroviral therapy

Preparation for childbirth
Collective sessions
Organizing group sessions (10-15 women) helps promote exchanges between women,
promote the use of available services and address the following topics:
– Importance of being assisted by qualified personnel during childbirth.
– Objectives of prenatal consultations.
– Screening tests and preventive treatments recommended during pregnancy.
– Protection against vector insect bites: impregnated mosquito nets, covering
clothing, certain repellents, etc. depending on the context (e.g. malaria, dengue, chikungunya, zika).
– Danger signs during pregnancy, labor or delivery, importance of prompt
treatment.
– Use of the “delivery kit”h(according to the context).
– Objectives of the postnatal visit.
– Birth control.
Individual sessions
The individual sessions make it possible to take up the themes covered in the group sessions and to give advice adapted to the individual medical and social situation.
The topics depend on the stage of the pregnancy and the specific situation of
the woman (eg drug use, domestic violence, genital mutilation).
Individual sessions must in all cases provide for the individual birth plan
Birth plan
Determine with the patient a delivery plan taking into account her medical and social situation:
– Place of delivery: SONUB or SONUC structures depending on the course of the pregnancy and the history.
– Provisions to be made: transport, family organization, etc.
Be rest assured at Hadassah Medical Centre, we treasure your health and that of your baby. We make sure your journey to motherhood is memorable
Contact us now at ![]() (+237 682 21 51 95 / 693 81 45 50 )
(+237 682 21 51 95 / 693 81 45 50 )
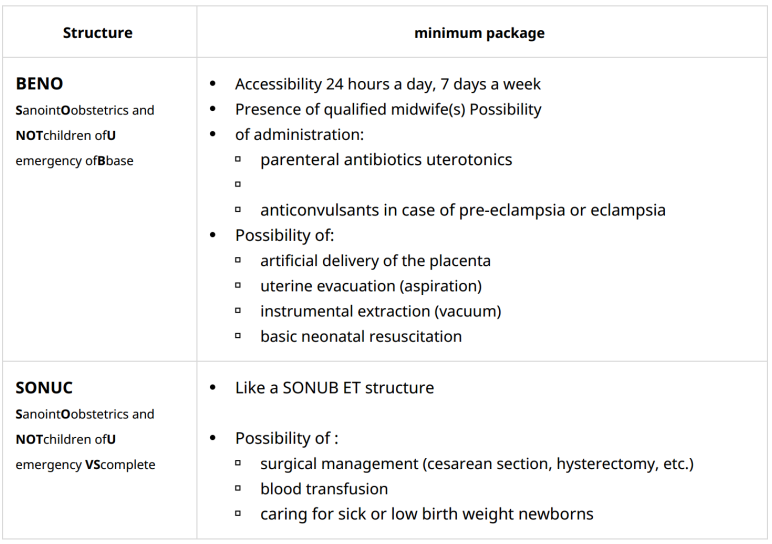
Table 1.7- Obstetric care facilities



